Introduction
Back pain is a common ailment that affects millions of people worldwide. It can range from a dull, constant ache to a sudden, sharp pain that makes movement difficult. Back pain is classified into two categories: acute and chronic. Acute back pain typically lasts for a few days to a few weeks, while chronic back pain persists for 12 weeks or longer, even after an initial injury or underlying cause has been treated.
Understanding the differences between acute and chronic back pain, as well as the appropriate diagnostic and treatment approaches, is essential for effective management and relief.
Diagnosing Acute and Chronic Back Pain
Medical History and Physical Examination
The diagnostic process for back pain begins with a thorough medical history and physical examination. During this evaluation, a healthcare provider will inquire about:
- The onset, duration, and nature of the pain.
- Any activities or injuries that may have triggered the pain.
- Associated symptoms such as numbness, weakness, or radiating pain.
- Previous episodes of back pain and treatments that were effective or ineffective.
- Medical conditions that may contribute to back pain, such as arthritis or osteoporosis.
A physical examination will involve assessing the spine’s alignment, range of motion, and areas of tenderness. The healthcare provider may also perform neurological tests to check reflexes, muscle strength, and sensation in the limbs.
Imaging Studies
Imaging studies are often used to provide a clearer picture of the structures within the back and identify any abnormalities. Common imaging techniques include:
- X-rays: Useful for detecting bone abnormalities, fractures, or degenerative changes in the spine.
- Magnetic Resonance Imaging (MRI): Provides detailed images of soft tissues, including discs, muscles, and nerves. MRI is particularly useful for identifying herniated discs, spinal stenosis, or tumors.
- Computed Tomography (CT) Scans: Offers detailed cross-sectional images of the spine and can be helpful in diagnosing bone problems or complex conditions.
- Bone Scans: Used to detect bone infections, fractures, or other bone disorders.
- Electromyography (EMG): Measures electrical activity in muscles and can help identify nerve compression or damage.
Treating Acute Back Pain
Acute back pain is often self-limiting, meaning it resolves on its own within a few weeks. Treatment focuses on relieving symptoms and maintaining function. Common approaches include:
Rest and Activity Modification
Short-term rest may be necessary to alleviate severe pain, but prolonged bed rest is discouraged as it can lead to stiffness and muscle weakness. Patients are encouraged to resume normal activities as soon as possible, avoiding movements that exacerbate pain.
Medications
Several medications can help manage acute back pain, including:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Such as ibuprofen or naproxen, to reduce pain and inflammation.
- Acetaminophen: For pain relief without the anti-inflammatory effects.
- Muscle Relaxants: Prescribed for short-term use to alleviate muscle spasms.
- Topical Analgesics: Creams or patches applied to the skin to relieve localized pain.
Physical Therapy
Physical therapy plays a crucial role in the treatment of acute back pain. Therapists can teach patients exercises to improve flexibility, strength, and posture, which can help prevent future episodes of pain. Techniques may include:
- Stretching Exercises: To improve flexibility and reduce muscle tension.
- Strengthening Exercises: Focused on the core muscles to support the spine.
- Manual Therapy: Techniques such as massage or spinal manipulation to alleviate pain and improve mobility.
- Education: On proper body mechanics and ergonomics to prevent re-injury.
Alternative Therapies
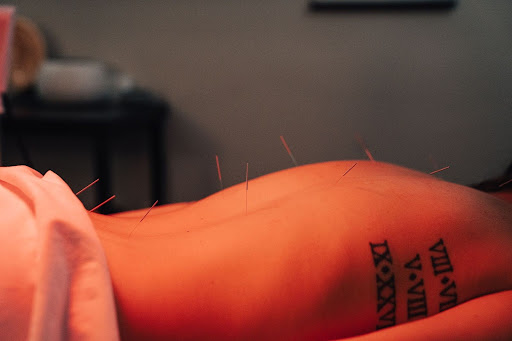
Some patients find relief from acute back pain through alternative therapies such as:
- Acupuncture: Involves inserting thin needles into specific points on the body to relieve pain.
- Chiropractic Care: Spinal adjustments performed by a chiropractor to improve alignment and reduce pain.
- Yoga and Pilates: Low-impact exercises that focus on stretching, strengthening, and improving posture.
Treating Chronic Back Pain
Chronic back pain requires a more comprehensive and multidisciplinary approach due to its persistent nature and potential impact on quality of life. Treatment aims to reduce pain, improve function, and enhance the patient’s ability to perform daily activities.
Medications
The management of chronic back pain may involve a combination of medications, including:
- NSAIDs and Acetaminophen: For ongoing pain relief.
- Antidepressants: Such as tricyclic antidepressants or serotonin-norepinephrine reuptake inhibitors (SNRIs), which can help with pain management and improve sleep.
- Anticonvulsants: Medications like gabapentin or pregabalin may be prescribed for nerve pain.
- Opioids: Reserved for severe pain that does not respond to other treatments, used with caution due to the risk of dependence and side effects.
- Topical Pain Relievers: Including lidocaine patches or capsaicin cream.
Physical Therapy and Exercise
Physical therapy remains a cornerstone of chronic back pain treatment. A tailored exercise program can help manage pain and improve function. Key components include:
- Aerobic Conditioning: Low-impact activities like walking, swimming, or cycling to improve overall fitness and reduce pain.
- Strength Training: Focusing on core muscles to support the spine and reduce strain.
- Flexibility Exercises: To maintain range of motion and prevent stiffness.
- Pain Education: Helping patients understand pain mechanisms and develop coping strategies.
Cognitive-Behavioral Therapy (CBT)
CBT is an effective psychological intervention for chronic back pain. It helps patients:
- Identify and Change Negative Thought Patterns: That can exacerbate pain and disability.
- Develop Coping Strategies: To manage pain and improve daily functioning.
- Set Realistic Goals: For activity and pain management.
Interventional Procedures
For patients who do not respond to conservative treatments, interventional procedures may be considered, including:
- Epidural Steroid Injections: To reduce inflammation and pain around the spinal nerves.
- Facet Joint Injections: To relieve pain originating from the small joints in the spine.
- Radiofrequency Ablation: Uses heat to disrupt nerve signals and reduce pain.
- Spinal Cord Stimulation: Involves implanting a device that delivers electrical impulses to the spinal cord to interfere with pain signals.
Surgery
Surgery is typically considered a last resort when other treatments have failed and the patient has severe, debilitating pain or significant neurological deficits. Common surgical options include:
- Discectomy: Removal of a herniated disc that is compressing a nerve.
- Laminectomy: Removal of part of the vertebra to relieve pressure on the spinal cord or nerves.
- Spinal Fusion: Joining two or more vertebrae to stabilize the spine.
- Artificial Disc Replacement: Replacing a damaged disc with an artificial one to maintain motion at the spinal segment.
Prevention of Back Pain
Preventing back pain involves lifestyle changes and strategies to reduce the risk of injury. Key preventive measures include:
Regular Exercise
Engaging in regular physical activity strengthens the muscles that support the spine, improves flexibility, and enhances overall fitness. Activities such as walking, swimming, and yoga are particularly beneficial.
Proper Body Mechanics
Learning and practicing proper body mechanics can help prevent back injuries. This includes:
- Lifting Techniques: Using the legs rather than the back to lift heavy objects.
- Posture: Maintaining good posture while sitting, standing, and sleeping.
- Ergonomics: Adjusting workstations to reduce strain on the back.
Healthy Weight
Maintaining a healthy weight reduces the strain on the back and minimizes the risk of developing back pain. A balanced diet and regular exercise are essential for weight management.
Stress Management
Chronic stress can contribute to muscle tension and back pain. Techniques such as mindfulness, meditation, and relaxation exercises can help manage stress levels.
Conclusion
Back pain, whether acute or chronic, requires a comprehensive approach to diagnosis and treatment. By understanding the underlying causes and employing a combination of medical, physical, and psychological strategies, individuals can effectively manage their pain and improve their quality of life. Preventive measures and lifestyle modifications play a crucial role in reducing the risk of back pain and promoting long-term spinal health.