Every human being experiences pain, which acts as a crucial warning system and defense mechanism. But when chronic pain persists longer than anticipated, it can become a crippling illness that affects millions of people globally. Scientific discoveries have expanded our knowledge of the mechanisms underlying pain, resulting in novel therapeutic approaches that provide hope and relief to those who suffer from chronic pain. This article will discuss the science of pain, new discoveries about pain pathways, and innovative pain treatments that are transforming the field of pain management.
The Intricacy of Pain
Pain is a complex phenomenon that is impacted by social, psychological, and biological elements. It involves complex neural system functions such as sensory perception, pain signal transmission, modulation, and brain interpretation. Comprehending the intricacy of pain is crucial in order to formulate efficacious therapeutic approaches that aim to address the fundamental mechanisms influencing the experience and endurance of pain.
1. Pain Types
Acute pain is the body’s protective reaction, alerting it to possible danger. It usually results from tissue damage or injury. Acute discomfort often subsides quickly as the underlying reason heals.
Chronic pain is defined as pain that lasts longer than the average healing period and can be caused by a number of things, such as inflammation, musculoskeletal problems, nerve damage, or underlying medical issues. Because chronic pain is complicated, specific treatment methods are frequently needed.
2. Anxiety Routes
Peripheral Nervous System (PNS): Specialized nerve endings known as nociceptors, which recognize potentially dangerous stimuli like heat, pressure, or chemicals, are responsible for initiating pain signals. The spinal cord receives these messages from sensory nerves.
Central Nervous System (CNS): Before pain impulses reach the brain, they are first processed and modified in the spinal cord. A part of pain perception that is sensory, emotional, and cognitive is the brain’s interpretation of these information.
3. The Regulation of Pain by Neurotransmitters
Endogenous Opioids: Endorphins and enkephalins are naturally occurring chemicals produced by the body that bind to opioid receptors in the brain and spinal cord to modulate pain signals and cause analgesic effects.
Serotonin and Norepinephrine: These neurotransmitters are involved in mood control, descending pain inhibition pathways, and pain modulation.
4. Pain Sensitization and Neuroplasticity
Neuroplastic Changes: Sensitization of pain pathways, amplification of pain signals, and modifications in synaptic transmission are just a few of the neuroplastic changes that chronic pain can cause in the nervous system. These changes can contribute to persistent pain states.
Central Sensitization: This phenomenon brings on increased pain sensitivity, allodynia (pain from non-painful stimuli), and hyperalgesia (increased pain response) in illnesses such as fibromyalgia, neuropathic pain, and complex regional pain syndrome (CRPS).
Current Developments in the Study of Pain
Recent scientific discoveries have expanded our knowledge of the mechanics underlying pain, opening the door to novel therapies and interventions that target certain pain pathways and provide long-lasting relief. Key areas of pain research progress include the following:
1. Pain and Genetics
Genetic variants: Studies have shown that certain genetic variants affect how people perceive pain, how sensitive they are to pain, and how they react to painkillers. Comprehending individual genetic profiles can inform tailored pain management strategies.
Epigenetics: Alterations in DNA and histones can affect the expression of genes linked to pain perception, inflammation, and neurogenesis. This information can provide light on possible targets for treatment.
2. Pain Mapping and Neuroimaging
Functional MRI (fMRI): With the use of sophisticated imaging techniques, researchers may map the brain regions involved in pain perception, emotion, and cognition as well as see brain activity linked to the processing of pain.
Neuroimaging Biomarkers: Patterns of brain connections, structural alterations, and neurotransmitter levels are examples of biomarkers obtained from neuroimaging data that provide diagnostic and prognostic information as well as direct treatment selection and monitoring.
3. Sensory Pathways of Pain
Transient Receptor Potential (TRP) Channels: TRP channels are involved in the transmission of pain and sensory perception. Certain drugs or therapies that target TRP channels have the potential to regulate pain signals and reduce symptoms.
Ion Channel Modulators: Substances that alter the sodium, potassium, and calcium channels—ion channels implicated in the transmission of pain—may be used as targets for cutting-edge analgesic treatments.
4. The Immune System and Neuroinflammation
Neuroinflammatory Pathways: Immune cells, cytokines, and inflammatory mediators in the nervous system are all involved in neuroinflammation, which is frequently linked to chronic pain. Pain and inflammation may be decreased by focusing on neuroinflammatory pathways.
Immunomodulation: To reduce pain-related inflammation and immunological dysregulation, new treatments, such as cytokine inhibitors, monoclonal antibodies, and cell-based therapies, outcomes by focusing on particular pain pathways and encouraging neuroplasticity. The following are a few instances of transformative therapies:
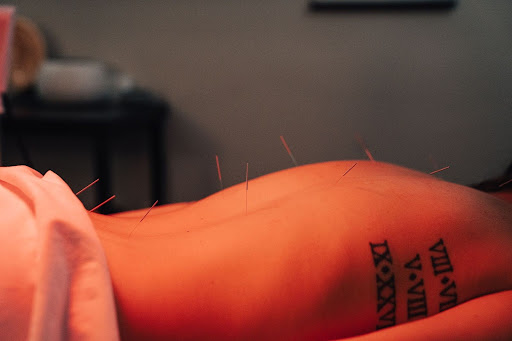
1. Treatments for Neuromodulation
concentrate on modifying immune responses.
Modern Approaches to Pain Management
Research on pain has led to the development of novel therapies and treatments that provide people with chronic pain fresh hope. These innovative methods enhance overall pain treatment
Spinal Cord Stimulation (SCS):
SCS is the process of implanting a device that stimulates the spinal cord with electrical impulses in order to modulate pain signals and alleviate chronic pain problems such complex regional pain syndrome (CRPS), failed back surgery syndrome, and neuropathic pain.
Peripheral Nerve Stimulation (PNS):
PNS uses electrical stimulation to target peripheral nerves in order to relieve peripheral neuropathies, neuropathic pain, and localized pain.
Deep Brain Stimulation (DBS): To treat illnesses including Parkinson’s disease, dystonia, and persistent neuropathic pain, DBS entails implanting electrodes in particular brain regions to control neural activity.
2. Personalized Medicine and Pharmacogenomics
Genetic Testing: Pharmacogenomic testing can detect genetic variants that affect how the body reacts to painkillers. This information can be used to select the right prescription for each patient, optimize dosage, and prevent negative drug reactions.
Precision Medicine: Treatment strategies for pain are customized based on individual factors such as metabolic profiles, genetic predispositions, and response to treatment. Precision medicine approaches incorporate genetic, genomic, and clinical data.
3. Biologics and Regenerative Medicine
Platelet-Rich Plasma (PRP) Therapy:
In musculoskeletal disorders such osteoarthritis, tendinitis, and ligament injuries, PRP injections use concentrated platelets from the patient’s blood to promote tissue healing, lower inflammation, and enhance pain and function.
Stem Cell Therapy: In order to treat chronic pain disorders, stem cell-based therapies use the regenerative capacity of stem cells to modify immune responses, heal damaged tissues, and encourage tissue regeneration.
4. Digital therapeutics with virtual reality (VR)
VR for Pain Distraction: VR technology offers immersive experiences that help patients relax, cope with anxiety, and block out pain. As such, it’s a useful tool for managing pain during surgeries, recovery periods, and treatments for chronic pain.
Digital therapeutics: Interactive tools, mindfulness exercises, cognitive-behavioral therapies, and instructional materials for pain self-management, monitoring, and support are available on digital platforms and applications.
In summary
Recent years have seen amazing progress in the study of pain, from deciphering the intricate pathways underlying pain to creating ground-breaking therapies that provide people with chronic pain new hope and opportunities. A deeper understanding of pain causes, individualized treatments, interdisciplinary teamwork, and cutting-edge technologies are all contributing to the evolution of pain management into more efficient, focused, and patient-centered care. Future research promises to improve our understanding of pain management, improve people’s quality of life, and provide better solutions for people dealing with the complicated issues associated with chronic pain.